BLOG
Step into Your Power. Learn, Transform, Thrive in Life Transitions. Embrace Your Best Self.

What are Haemorrhoids? Why are they more common after Menopause?
You might have heard people talk about piles or haemorrhoids, often with a bit of embarrassment. Society tends to keep discussions about 'down there' private. Whether you're dealing with symptoms or just curious, understanding haemorrhoids and their link to menopause can be helpful.
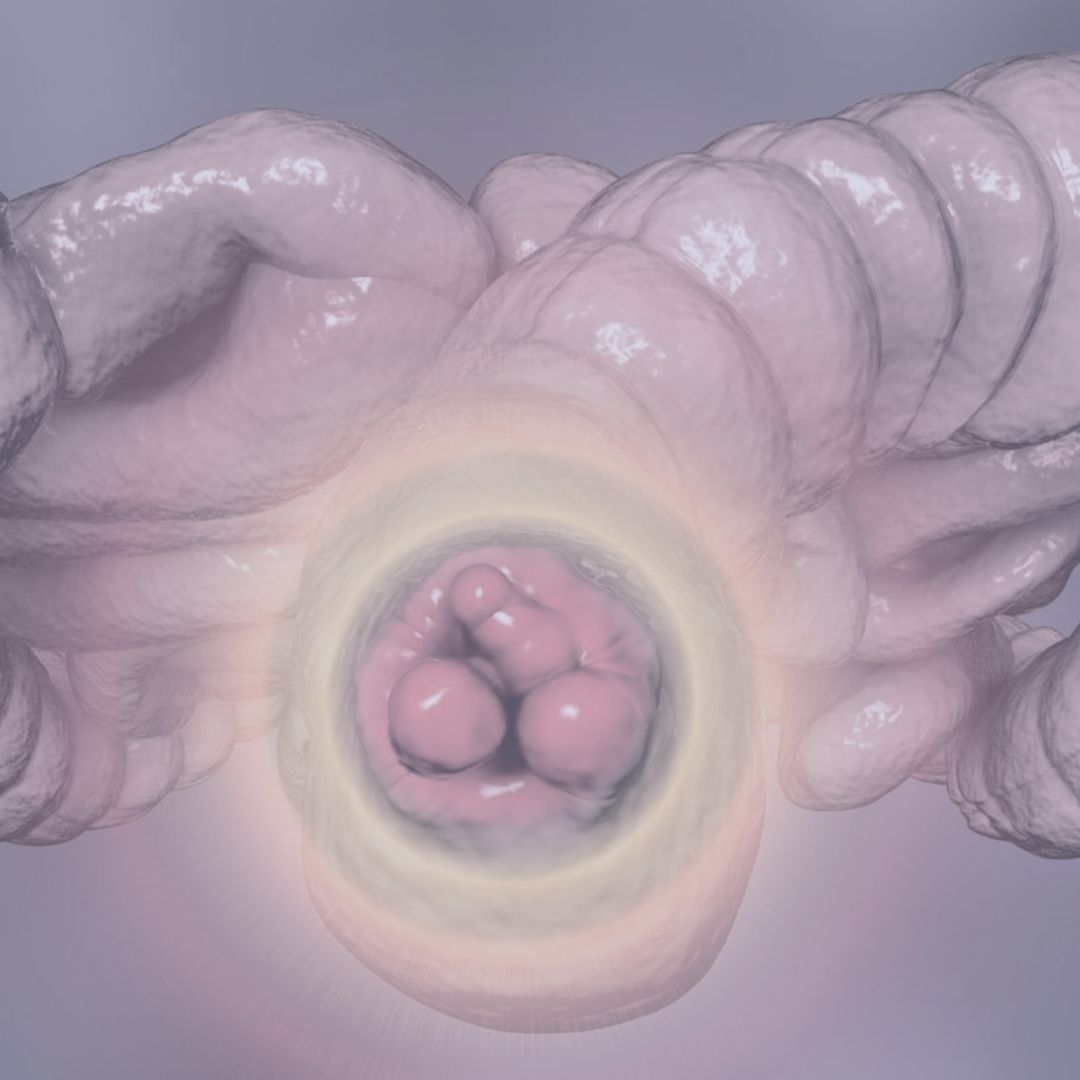
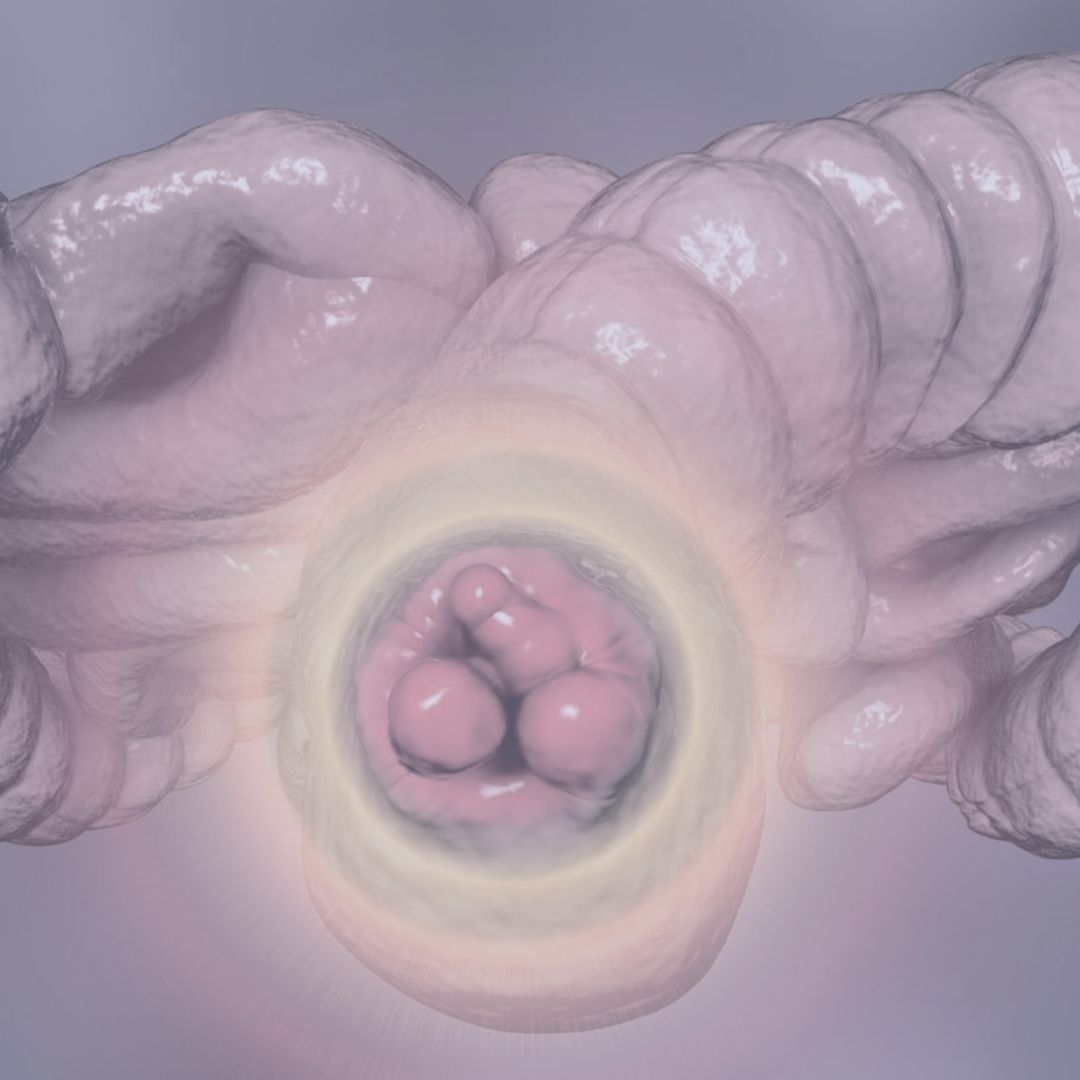
What Are Haemorrhoids?
Haemorrhoids, or piles, are swollen tissues and veins in the anal canal. They contain blood vessels, muscle, and elastic fibres. These can vary in size, with many women experiencing internal haemorrhoids located 2-4 cm above the anus.
Causes of Haemorrhoids
Haemorrhoids develop due to increased pressure in the rectum and anus. This pressure can come from:
- Chronic constipation
- Chronic diarrhoea
- Lifting heavy weights
- Pregnancy
- Straining during bowel movements
- Obesity
This pressure causes the blood vessels in these areas to stretch and swell.
The likelihood of getting haemorrhoids increases as you age.
Why Are Haemorrhoids More Common After Menopause?
After menopause, a drop in oestrogen levels can lead to haemorrhoids. Oestrogen helps support the walls of the rectum and vagina and has anti-inflammatory properties. Without enough oestrogen, tissues are more prone to inflammation. Menopause can also affect digestion and bowel movements, leading to constipation or diarrhoea, which can contribute to haemorrhoids.
Symptoms of Haemorrhoids
Common symptoms include:
- Hard, painful lumps around the anus, possibly containing clotted blood
- Feeling of fullness in the rectum after a bowel movement
- Bright red blood after a bowel movement (always check with a doctor for rectal bleeding)
- Itchy, red, and sore area around the anus
- Pain when passing stools
Grades of Haemorrhoids
Grade 1: Small inflammations inside the anus
Grade 2: Larger inflammations that may come out during bowel movements but go back in easily
Grade 3: Prolapsed haemorrhoids that can be pushed back in
Grade 4: Prolapsed haemorrhoids that cannot be pushed back in and need medical treatment
External haemorrhoids can form lumps that become itchy and painful, especially if a blood clot forms. Severe pain requires medical attention.
Treatment for Haemorrhoids
Most haemorrhoids, especially lower grades, resolve on their own. To help speed up recovery and prevent recurrence:
- Reduce Constipation and Straining: Drink 1.5-2 litres of water daily, eat plenty of fibre from fruits and vegetables, and avoid processed foods. Regular gentle exercise can help stimulate bowel movements.
- Lose Weight: If you're overweight, losing weight can reduce pressure on your rectum and anus.
- Toilet Habits: Sit correctly on the toilet to avoid straining.
Medical Treatments
- Over-the-counter creams
- Steroid creams
- Laxatives
- Surgery
If conservative treatments fail, 1 in 10 people may need surgery. Various techniques are available, and it's important to discuss options and potential side effects with a surgeon.
Prevention
The best way to deal with haemorrhoids is to prevent them. Maintain healthy bowel movements and avoid straining. Don’t be embarrassed to seek help and always get any rectal bleeding checked out by a doctor.
If you would like more support on your journey, check out my services on my website.

Sign up for our newsletter.
BLOG
Step into Your Power.
Learn, Transform, Thrive in Life Transitions.
Embrace Your Best Self.

What are Haemorrhoids? Why are they more common after Menopause?
You might have heard people talk about piles or haemorrhoids, often with a bit of embarrassment. Society tends to keep discussions about 'down there' private. Whether you're dealing with symptoms or just curious, understanding haemorrhoids and their link to menopause can be helpful.
What Are Haemorrhoids?
Haemorrhoids, or piles, are swollen tissues and veins in the anal canal. They contain blood vessels, muscle, and elastic fibres. These can vary in size, with many women experiencing internal haemorrhoids located 2-4 cm above the anus.
Causes of Haemorrhoids
Haemorrhoids develop due to increased pressure in the rectum and anus. This pressure can come from:
- Chronic constipation
- Chronic diarrhoea
- Lifting heavy weights
- Pregnancy
- Straining during bowel movements
- Obesity
This pressure causes the blood vessels in these areas to stretch and swell.
The likelihood of getting haemorrhoids increases as you age.
Why Are Haemorrhoids More Common After Menopause?
After menopause, a drop in oestrogen levels can lead to haemorrhoids. Oestrogen helps support the walls of the rectum and vagina and has anti-inflammatory properties. Without enough oestrogen, tissues are more prone to inflammation. Menopause can also affect digestion and bowel movements, leading to constipation or diarrhoea, which can contribute to haemorrhoids.
Symptoms of Haemorrhoids
Common symptoms include:
- Hard, painful lumps around the anus, possibly containing clotted blood
- Feeling of fullness in the rectum after a bowel movement
- Bright red blood after a bowel movement (always check with a doctor for rectal bleeding)
- Itchy, red, and sore area around the anus
- Pain when passing stools
Grades of Haemorrhoids
Grade 1: Small inflammations inside the anus
Grade 2: Larger inflammations that may come out during bowel movements but go back in easily
Grade 3: Prolapsed haemorrhoids that can be pushed back in
Grade 4: Prolapsed haemorrhoids that cannot be pushed back in and need medical treatment
External haemorrhoids can form lumps that become itchy and painful, especially if a blood clot forms. Severe pain requires medical attention.
Treatment for Haemorrhoids
Most haemorrhoids, especially lower grades, resolve on their own. To help speed up recovery and prevent recurrence:
- Reduce Constipation and Straining: Drink 1.5-2 litres of water daily, eat plenty of fibre from fruits and vegetables, and avoid processed foods. Regular gentle exercise can help stimulate bowel movements.
- Lose Weight: If you're overweight, losing weight can reduce pressure on your rectum and anus.
- Toilet Habits: Sit correctly on the toilet to avoid straining.
Medical Treatments
- Over-the-counter creams
- Steroid creams
- Laxatives
- Surgery
If conservative treatments fail, 1 in 10 people may need surgery. Various techniques are available, and it's important to discuss options and potential side effects with a surgeon.
Prevention
The best way to deal with haemorrhoids is to prevent them. Maintain healthy bowel movements and avoid straining. Don’t be embarrassed to seek help and always get any rectal bleeding checked out by a doctor.
If you would like more support on your journey, check out my services on my website.

Sign up for our newsletter.